When you walk into a doctor’s office for a routine checkup, you expect your provider to know exactly what medication you need. But what if that decision isn’t made by one person alone? In today’s healthcare system, generic prescribing is no longer just a doctor’s call-it’s a team effort. And that shift is changing how patients get treated, save money, and avoid dangerous drug interactions.
Why Team-Based Care Matters for Medications
For years, prescribing was seen as a solo act. The physician reviewed symptoms, checked lab results, wrote a script, and sent the patient on their way. But this model broke down when patients started juggling five, six, or even ten medications for diabetes, high blood pressure, cholesterol, and arthritis. Medication errors rose. Costs spiked. Patients got confused. And many stopped taking their pills altogether. Enter team-based care. It’s not a buzzword-it’s a proven system where pharmacists, nurses, care coordinators, and physicians work together, with the patient at the center. The National Academy of Medicine formally defined this in 2017, but the roots go back to the 2001 Institute of Medicine report that called out fragmented care as a major threat to patient safety. The real turning point came with Medicare Part D in 2003, which required pharmacies to offer Medication Therapy Management (MTM) for high-risk patients. That’s when pharmacists went from dispensers to active decision-makers.Who’s on the Team and What Do They Do?
A team-based approach to generic prescribing isn’t just adding more people to the room. It’s about clear roles:- Physicians handle complex diagnoses and overall treatment plans. They approve final prescriptions but don’t manage daily med details.
- Pharmacists are the medication experts. They run comprehensive reviews, spot duplicates, check for interactions, and recommend generic alternatives that work just as well. Studies show they reduce medication errors by 67% when fully integrated.
- Nurses and Medical Assistants monitor chronic conditions like blood pressure or blood sugar. They catch early signs that a medication isn’t working or causing side effects.
- Care Coordinators make sure everyone’s on the same page. They update electronic records, schedule follow-ups, and help patients navigate insurance hurdles.
How Generic Prescribing Works in a Team Setting
Generic drugs aren’t cheap knockoffs. They’re identical in active ingredient, dosage, and effectiveness to brand-name versions. The difference? Price. A generic statin can cost $5 a month instead of $150. But switching isn’t automatic. Patients worry: "Will this work?" "Is it safe?" "Will my doctor think I’m cheap?" That’s where the team steps in. A pharmacist doesn’t just swap a pill. They explain it. They show data. They answer questions. And they document the change clearly in the record so the doctor knows why the switch happened. Medicare Part D’s MTM program requires pharmacists to perform nine specific services, including:- Reviewing all medications for safety and effectiveness
- Identifying drug interactions
- Recommending generic alternatives
- Teaching patients how to take meds correctly
- Coordinating care with other providers
Where It Works Best-and Where It Doesn’t
Team-based care shines where medications are complex and long-term: diabetes, heart failure, high blood pressure, asthma, and high cholesterol. These conditions need constant monitoring, frequent adjustments, and patient education. A single visit every three months isn’t enough. But in urgent care? When someone comes in with a sudden chest pain or infection? Team-based care isn’t practical. You need fast decisions, not committee votes. That’s where the physician still leads. The key is knowing when to use the team. High-risk patients-those on five or more medications, with three or more chronic conditions, and annual drug costs over $4,000-are the perfect candidates. In 2023, Medicare expanded eligibility to include people on just four medications, adding over 4 million more people to these programs.Real Challenges in Real Clinics
It’s not all smooth sailing. Setting up a team-based system costs practices $85,000 to $120,000 upfront. That’s a big hit for small clinics. Some doctors resist giving up control. "I’ve been prescribing for 20 years. Why do I need a pharmacist telling me what to do?" There are also tech problems. If the electronic health record doesn’t talk between the doctor’s system and the pharmacy’s, information gets lost. One study found 12% of negative patient reviews mentioned "communication breakdowns" between team members. And reimbursement is still a mess. Only 41% of team-based medication services are paid at a level that covers their true cost. That’s why many clinics struggle to keep pharmacists on staff full-time. But the biggest hurdle? Time. One physician on Doximity said it took him 2.5 extra hours a week just to adjust to the new workflow-until they added daily 15-minute huddles and standardized checklists. That’s when things clicked.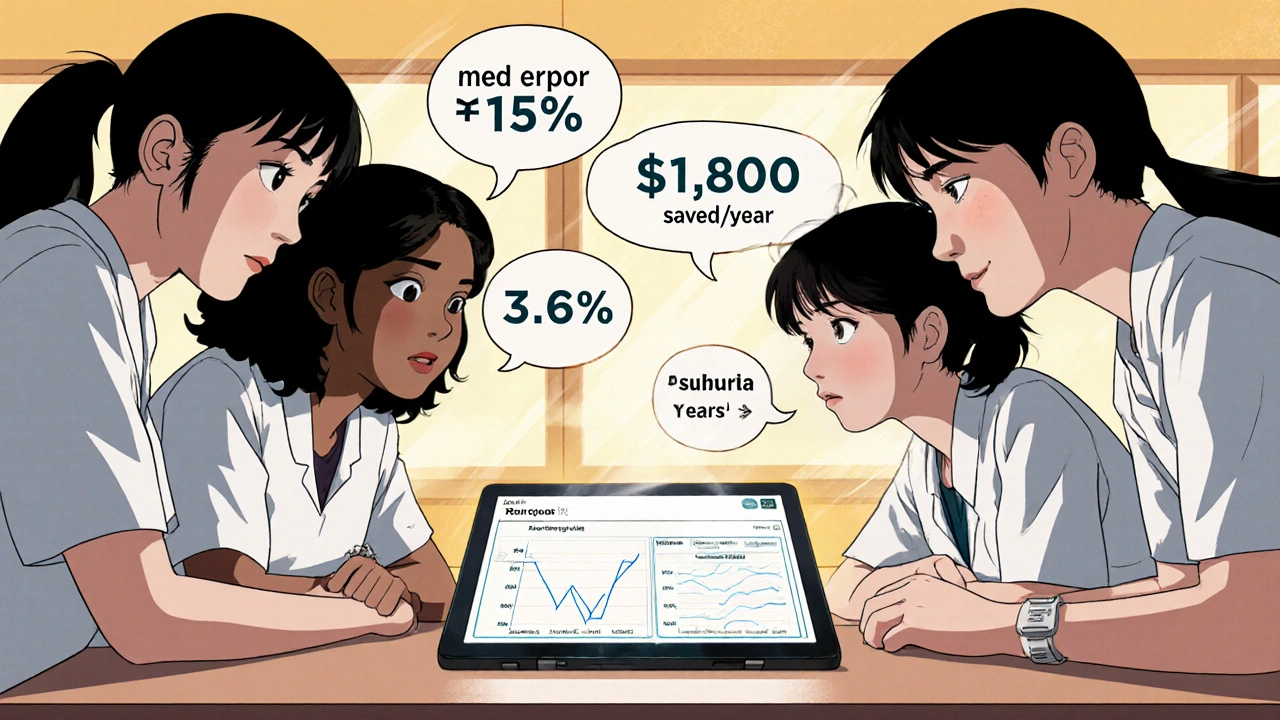
What Successful Teams Do Differently
The clinics that make this work have three things in common:- Daily huddles-15 minutes, every morning. Quick updates on who needs med reviews, who’s having side effects, who’s due for a refill.
- Collaborative Practice Agreements (CPAs)-formal documents that let pharmacists adjust doses or switch to generics under agreed-upon rules, without waiting for doctor approval every time.
- Integrated EHRs-a single system where every team member sees the same updates in real time. This cuts medication reconciliation time by 35%.
The Future: AI, Telepharmacy, and More Access
Team-based care isn’t slowing down-it’s accelerating. Telepharmacy services grew 214% between 2020 and 2023. Now, patients in rural towns can get a virtual med review from a pharmacist without driving 40 miles. Even more exciting? Artificial intelligence. Mayo Clinic’s pilot program used AI to suggest generic alternatives based on patient history, insurance coverage, and drug interaction risks. The result? 22% more appropriate generic switches and a 9.3% drop in adverse events. And the numbers don’t lie. The global team-based care market is set to hit $53.2 billion by 2027. Medicare Advantage plans are now required to offer full medication management. Sixty-eight percent of large health systems have already adopted it.What This Means for You
If you’re on multiple medications, especially for chronic conditions, ask your doctor: "Is there a pharmacist on my care team?" If not, request one. You have the right to a full medication review. If you’re a provider, don’t see team-based care as extra work. See it as a way to reduce burnout. Physicians in one Reddit thread reported a 30% drop in time spent on med management after bringing in pharmacists. That’s more time for complex cases-and less frustration. Generic prescribing isn’t about cutting corners. It’s about using the right tool for the job. And when a team of experts works together-with the patient’s goals in mind-it’s not just cheaper. It’s safer. It’s smarter. And it’s the future of care.Can pharmacists legally prescribe generic medications in team-based care?
Yes, but only under formal Collaborative Practice Agreements (CPAs) that are approved by state law and the supervising physician. These agreements allow pharmacists to initiate, adjust, or switch medications-including to generics-within defined clinical protocols. For example, a pharmacist can switch a patient from brand-name lisinopril to generic lisinopril without re-consulting the doctor, as long as the patient’s blood pressure is stable and there are no contraindications.
Do generic drugs work as well as brand-name drugs?
Absolutely. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for purity, stability, and bioavailability. The only differences are in inactive ingredients like fillers or dyes, which rarely affect effectiveness. Studies consistently show no clinical difference in outcomes between generics and brand-name drugs for conditions like hypertension, diabetes, and high cholesterol.
Who qualifies for Medication Therapy Management (MTM) under Medicare Part D?
As of 2023, Medicare Part D beneficiaries qualify for MTM if they have three or more chronic conditions (like diabetes, heart failure, or COPD), take five or more Part D-covered medications, and have annual drug costs exceeding $4,000. In 2023, the threshold was lowered to four medications for certain high-risk groups, expanding eligibility to over 4 million additional people.
Why aren’t all doctors using team-based care for prescribing?
Cost and culture. Setting up the system requires upfront investment in staff, training, and technology-often $100,000 or more. Many physicians are used to working alone and worry about losing control. Reimbursement is also inconsistent; only 41% of team-based medication services are paid at full cost. Small practices, in particular, struggle to justify the expense without guaranteed returns.
Can team-based care reduce hospital readmissions?
Yes. Research from ThoroughCare shows team-based medication management reduces hospital readmissions by 17.3%. This happens because pharmacists catch dangerous drug interactions, ensure patients understand how to take their meds, and prevent avoidable complications like kidney damage from NSAIDs or low blood pressure from too many heart meds. Better medication management means fewer ER visits and fewer trips back to the hospital.

Curtis Ryan
November 29, 2025 AT 00:51OMG THIS IS SO GOOD I WAS JUST TALKING TO MY PHARMACIST LAST WEEK AND SHE SAID SHE CAN SWITCH MY BP MED TO GENERIC AND SAVE ME $200 A MONTH!! I THOUGHT SHE WAS JUST BEING NICE BUT SHE ACTUALLY DID IT!! THANKS FOR SHARING THIS!! 🙌❤️
Rajiv Vyas
November 29, 2025 AT 07:24team-based care? more like government-controlled pharmacy dictatorship. next they'll be forcing us to take generic aspirin made in china. who even runs these clinics? bureaucrats? lol. i'll stick with my doctor who knows what he's doing. 🤡
farhiya jama
November 30, 2025 AT 07:12ugh i hate when people act like this is some revolutionary idea. my mom's been on 8 meds for 15 years and no one ever explained anything to her. now they just hand her a pill bottle and say 'you're fine.' this whole system is broken. why do i even bother?
Astro Service
December 1, 2025 AT 08:16pharmacists prescribing? no way. this is socialism creeping into healthcare. we don't need some guy in a white coat telling my doctor what to do. america built this system on individual responsibility. not team huddles. get real.
DENIS GOLD
December 1, 2025 AT 11:44oh wow, so now pharmacists are doctors? next they'll let the barista prescribe insulin. hilarious. i bet these 'studies' were funded by big generic pharma. who's really saving money here? not you.
Ifeoma Ezeokoli
December 3, 2025 AT 03:10my cousin in Lagos just got her first med review through a mobile pharmacy van-no doctor needed. it was life-changing. i think this model should be global, not just for rich countries. we need more of this, not less. 🌍❤️
Daniel Rod
December 4, 2025 AT 11:04i've been thinking a lot about this lately. we treat medicine like a solo sport, but healing is a community thing. the body doesn't care who writes the script-it just wants to be understood. maybe the real innovation isn't the team... it's remembering we're all human. 🤝💙
gina rodriguez
December 5, 2025 AT 12:46i work in a clinic that does this and it’s been amazing. patients are less anxious, we make fewer mistakes, and honestly? my burnout dropped. it’s not perfect, but it’s way better than the old way. small wins matter.
Sue Barnes
December 6, 2025 AT 16:36if your doctor doesn't know what they're doing, you're not a patient-you're a liability. pharmacists aren't doctors. let them count pills and leave the prescribing to those who went to med school. this is dangerous.
jobin joshua
December 7, 2025 AT 10:17bro i got my meds switched last month and my wife said i stopped yelling at the TV. maybe generics help with mood too? 😂💊
Daniel Rod
December 9, 2025 AT 09:34that’s actually beautiful. sometimes the medicine isn’t in the pill-it’s in the peace of mind. 🙏❤️