If you’ve ever felt like the room is spinning, even when you’re sitting still, and then got a pounding headache right after - you’re not alone. This isn’t just a bad migraine or a random dizzy spell. It’s vestibular migraine, a neurological condition that’s more common than most people realize. About 1 in 100 adults experience it, and women are more than three times as likely to be affected. Yet, most people wait over a year before getting the right diagnosis. Too often, doctors mistake it for inner ear problems or stress-induced dizziness. The truth? Vestibular migraine isn’t about your ears. It’s about your brain.
What Vestibular Migraine Really Is
Vestibular migraine isn’t just a headache with dizziness. It’s a specific brain-based disorder where the same nerve pathways that trigger migraine pain also disrupt your balance system. The vestibular system - located in your inner ear and connected to your brainstem - helps you stay upright and oriented. When migraine activity spreads to this area, it causes vertigo, unsteadiness, or a floating sensation. These episodes can last from a few minutes to three full days.
What makes it tricky is that you don’t always get a headache. In fact, about half of all vestibular migraine attacks happen without any head pain at all. Instead, you might feel nauseous, sensitive to light or sound, or see flashing lights before your balance goes haywire. This is why so many people end up seeing ENT specialists first, only to be told they have “benign vertigo” or “inner ear issues.” But if your dizziness comes with migraine triggers - like stress, skipped meals, or certain foods - it’s likely vestibular migraine.
The International Headache Society officially recognized this condition in 2013. Since then, research has shown it’s the most common cause of spontaneous vertigo in adults. Yet, 40% of cases are still misdiagnosed - often as BPPV (a harmless inner ear crystal problem) or Ménière’s disease (a rare inner ear fluid disorder). Getting the diagnosis right is the first step to stopping the cycle.
What Triggers Your Attacks?
Knowing your triggers is like having a map to avoid storms. For most people with vestibular migraine, attacks don’t come out of nowhere. They’re pulled by predictable patterns. A 2021 survey of over 850 patients found the top triggers:
- Stress (82%)
- Sleep disruption (76%)
- Weather changes (68%)
- Caffeine (54%)
- Alcohol (49%)
- Aged cheeses, processed meats, and MSG (38%)
Some triggers are obvious - like drinking wine on a Friday night and waking up dizzy the next morning. Others are sneaky. Skipping lunch? That’s a trigger. Staying up past midnight watching TV? That’s a trigger. Even a change in barometric pressure before a storm can set off an attack. The key is tracking. Keep a simple diary for six to eight weeks. Note what you ate, how much you slept, your stress level, and when the dizziness hit. Patterns will emerge.
One patient I know tracked her attacks for months and realized she only got dizzy after eating chocolate - not because of the sugar, but because of the tyramine in dark cocoa. Once she cut it out, her episodes dropped by 60%. Small changes matter.
How to Stop an Attack in Its Tracks
When a vestibular migraine attack hits, your brain is in overload. Your goal isn’t to “push through” - it’s to quiet the storm. Here’s what works:
- Dark, quiet room: Light and sound make vertigo worse. Get into a dark room, lie down, and close your eyes. Studies show this reduces symptom severity by 35% within an hour.
- Hydration: Drink 2 liters of water during an attack. Dehydration worsens both migraine and dizziness.
- Medications for vertigo: Prochlorperazine (5-10 mg) is the most effective acute treatment for dizziness, resolving symptoms in 68% of cases within two hours. Ondansetron helps with nausea and vomiting.
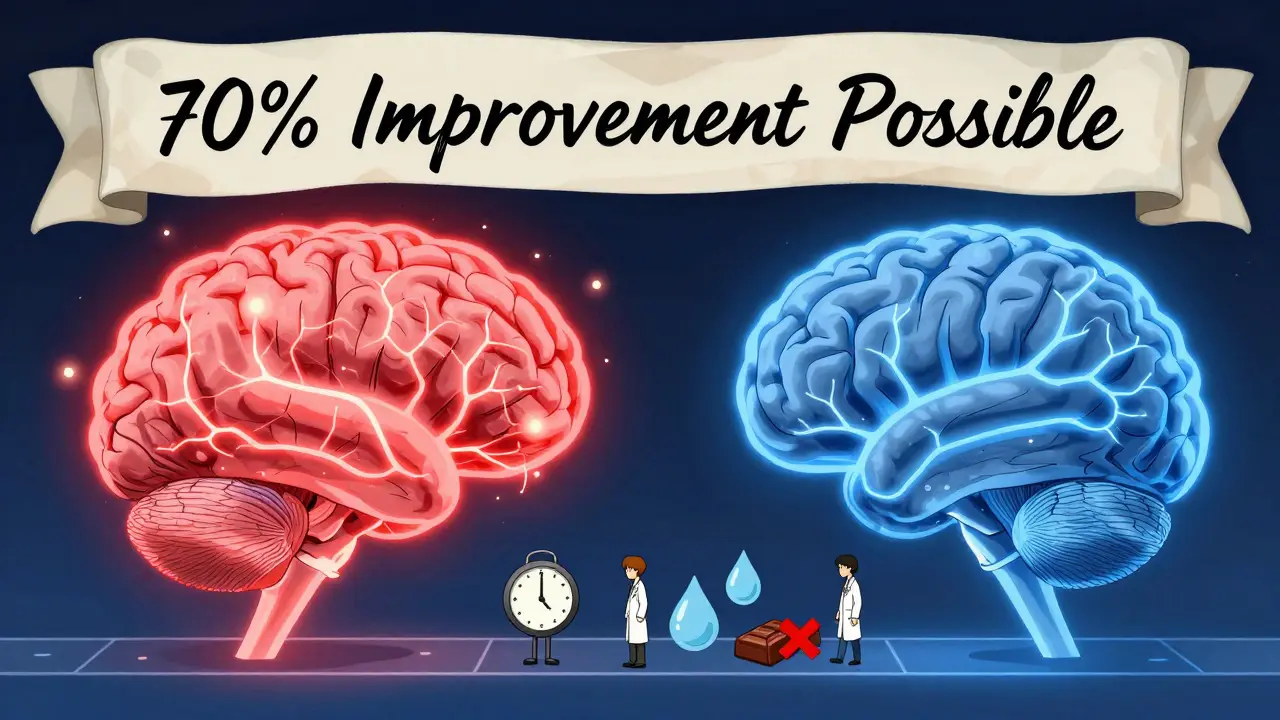
- Medications for headache: If you have head pain, sumatriptan (50-100 mg) works for 70% of people within two hours. Ibuprofen or naproxen can help too, but they’re less reliable for pure vestibular attacks.
- Avoid benzodiazepines: Drugs like diazepam or lorazepam may calm you down, but they can interfere with your brain’s natural ability to recover balance. Long-term use leads to dependency and delays recovery.
Many people try over-the-counter motion sickness pills like meclizine. They don’t work well for vestibular migraine - they just make you groggy without stopping the root cause. Focus on treatments that target the migraine pathway, not just the dizziness.
Preventing Attacks Before They Start
If you have more than four attacks a month, you need prevention - not just rescue. The goal is to reduce the frequency and severity so you can live without fear of the next episode.
First-line preventives are proven and widely used:
- Propranolol or metoprolol: These beta-blockers reduce attack frequency by 50% in 62% of patients. Start low - 40 mg daily - and increase slowly.
- Amitriptyline: A low-dose tricyclic antidepressant (10-25 mg at night) works surprisingly well for both migraine and dizziness. Side effects? Drowsiness, dry mouth - but many tolerate it better than expected.
- Verapamil: A calcium channel blocker, often used for high blood pressure, also helps stabilize brain activity. Dose: 120-240 mg daily.
- Topiramate: Reduces attacks by over 50% in 54% of patients, but can cause brain fog or tingling. Not ideal if you work with detail or drive often.
In Europe, flunarizine is a top choice. It’s not approved in the U.S., but many neurologists prescribe it off-label. A 2017 Cochrane review found it cut attacks nearly in half compared to placebo.
For those who want to avoid pills, supplements have solid evidence:
- Magnesium (600 mg daily): Helps calm overactive nerves. Best form: magnesium glycinate.
- Riboflavin (400 mg daily): Vitamin B2. Studies show it reduces attack frequency by 30-40%.
- Coenzyme Q10 (300 mg daily): Supports mitochondrial energy in brain cells. Works well with magnesium.
The CHARM study in 2015 showed these three together reduced attacks as effectively as some prescription drugs - with almost no side effects.
Vestibular Rehabilitation: The Game Changer
Here’s the part most people overlook: your brain can relearn balance. Vestibular rehabilitation therapy (VRT) isn’t just for people who’ve had strokes or inner ear damage. It’s for anyone whose brain has learned to overreact to movement.
Vestibular rehab involves simple, guided exercises - like focusing on a fixed point while moving your head, or standing on one foot with eyes closed. These aren’t fancy machines or expensive equipment. They’re movements your brain needs to rewire itself. In the 2018 DIZZINESS trial, patients who did VRT for eight weeks improved their dizziness scores by 40%. In a 2020 study, 78% of patients who completed 12 sessions reported over 50% symptom reduction.
Start with a physical therapist trained in vestibular rehab. Most insurance covers it. Do the exercises daily, even when you feel fine. It’s like physical therapy for your balance system. Over time, your brain stops misinterpreting normal motion as danger.
What Doesn’t Work - And Why
Many treatments for other dizziness conditions fail miserably for vestibular migraine.
- Diuretics (like hydrochlorothiazide): Used for Ménière’s disease, they help only 20% of VM patients - because VM isn’t about fluid buildup.
- Corticosteroids: Used for vestibular neuritis, they have only a 30% success rate in VM. Inflammation isn’t the issue.
- Long-term benzodiazepines: They numb the symptoms but stop your brain from healing. Patients who use them for months often end up more unsteady than before.
- Butterbur: Once popular for migraine prevention, it’s now banned in many countries due to liver damage risk. Avoid it.
The biggest mistake? Treating the dizziness like an ear problem. Vestibular migraine is a brain disorder. You need brain-targeted treatment.
When to See a Specialist
If you’ve had more than three unexplained dizzy episodes in a year - especially if they come with light sensitivity, nausea, or a history of migraines - see a neurologist who specializes in headaches or vestibular disorders. Don’t wait. Delaying treatment increases your risk of chronic dizziness by 30% within two years.
The best outcomes happen when you combine care: a neurologist for migraine prevention, an ENT to rule out inner ear issues, and a vestibular therapist for rehab. In 70% of successful cases, patients see at least two specialists working together.
And don’t be discouraged if the first medication doesn’t work. It often takes 2-3 tries to find the right one. One patient tried propranolol, then topiramate, then amitriptyline - and only the last one gave her back her life. Patience isn’t optional. It’s part of the treatment.
The Future Is Getting Brighter
There’s real progress on the horizon. In 2023, the FDA approved atogepant, a new migraine preventive that showed 56% effectiveness in vestibular migraine patients. Rimegepant, another new drug, cut vertigo days by nearly half in a 2022 trial. Non-invasive devices like gammaCore - which stimulates the vagus nerve through the neck - are now showing 45% reduction in dizziness.
Scientists are also working on biomarkers. A test called VEMP (vestibular-evoked myogenic potential) can detect abnormal brainstem responses in VM with 82% accuracy. Soon, diagnosis may be as simple as a 10-minute test - not a year of misdiagnosis.
For now, the tools we have work. Not perfectly. But well enough. With the right combination of trigger control, medication, and vestibular rehab, most people can reduce attacks by 70% or more. You don’t have to live in fear of the next spin. You just need the right plan.
Can vestibular migraine cause permanent hearing loss?
No, vestibular migraine does not cause permanent hearing loss. While some people report ringing in the ears (tinnitus) or muffled hearing during an attack, these symptoms are temporary and resolve after the episode ends. This is different from Ménière’s disease, which can lead to progressive hearing damage. If you have ongoing hearing changes, see an ENT to rule out other conditions.
Is vestibular migraine the same as BPPV?
No. BPPV (benign paroxysmal positional vertigo) is caused by loose crystals in the inner ear and triggers dizziness only when you change head position - like rolling over in bed or looking up. Vestibular migraine causes dizziness without positional triggers, often with migraine symptoms like light sensitivity or nausea. BPPV is treated with head maneuvers (Epley maneuver), while VM needs migraine-focused treatment. Misdiagnosing VM as BPPV leads to ineffective care.
Can stress really trigger vestibular migraine?
Yes - stress is the #1 trigger for vestibular migraine, reported by 82% of patients. It’s not just emotional stress. Physical stress like lack of sleep, overexertion, or even intense exercise can set off an attack. Managing stress with routines, sleep hygiene, and mindfulness doesn’t eliminate attacks, but it reduces their frequency and severity.
Are there any foods I should avoid?
Yes. Common food triggers include caffeine (coffee, tea, chocolate), alcohol (especially red wine), aged cheeses, processed meats with nitrates, MSG, and artificial sweeteners. Keep a food diary for 6-8 weeks to find your personal triggers. You don’t need to eliminate everything - just the ones that consistently lead to attacks.
How long does vestibular rehabilitation take to work?
Most people start noticing improvement after 4-6 weeks of daily exercises. Full benefits typically take 8-12 weeks. The key is consistency - doing the exercises even on days you feel fine. VRT retrains your brain to process balance signals correctly, which takes time. Skipping sessions delays results.
Can I still drive with vestibular migraine?
During an active attack, no - dizziness and visual sensitivity make driving unsafe. Between attacks, most people can drive safely. If you’ve had recent episodes, talk to your doctor. Some patients avoid driving during high-risk times (like after poor sleep or during weather changes). Never drive if you feel off-balance or nauseous.


fiona vaz
January 27, 2026 AT 17:01This post literally saved my life. I thought I was going crazy for two years until I found this. Now I track my sleep, skip the aged cheese, and do my VRT exercises daily. No more hiding in dark rooms. I’m actually planning a trip again. Thank you.
Sue Latham
January 29, 2026 AT 15:14Wow, you actually did your research. Most people just blame stress or ‘anxiety’ and pop Xanax like candy. Honestly? It’s refreshing to see someone who didn’t just Google ‘dizzy and headache’ and call it a day. You’re doing better than 90% of the internet.
John Rose
January 31, 2026 AT 08:05Thank you for the detailed breakdown. I’ve been seeing an ENT for vertigo for 14 months and was told it was ‘probably BPPV.’ Your point about the brainstem involvement and the 40% misdiagnosis rate is spot-on. I’m scheduling a neurology consult tomorrow. I’ll update if we find the right protocol.
Colin Pierce
February 2, 2026 AT 01:40I’m a physical therapist who specializes in vestibular rehab. Just wanted to say - the VRT section here is gold. I’ve had patients improve faster when they combine magnesium + riboflavin + daily head movements. One guy went from 5 attacks a week to 1 a month in 10 weeks. Don’t skip the exercises just because you feel okay. Your brain needs the repetition.
Mark Alan
February 3, 2026 AT 04:07OMG YES 🙌 I’ve been screaming this from the rooftops! My doctor told me to ‘take a chill pill’ and I was like NOPE. I cut out caffeine, started taking CoQ10, and now I’m hiking again. 🏔️💃 This is the most accurate thing I’ve read all year. THANK YOU!!!
Ambrose Curtis
February 5, 2026 AT 01:33listen. i’ve had this for 8 years. tried everything. propranolol made me feel like a zombie. topiramate gave me brain fog so thick i forgot my own birthday. then i found out i was allergic to MSG and tyramine. no more chinese food. no more red wine. no more processed crap. and guess what? my attacks dropped from 20 a month to 2. i didn’t need a pill. i just needed to stop poisoning myself. also - vrt works. do it even when you’re ‘fine.’ your brain is learning. be patient. it’s not magic. it’s biology.
jonathan soba
February 5, 2026 AT 04:05Interesting. But let’s be honest - how many of these ‘success stories’ are just placebo effects? You mention a 2017 Cochrane review on flunarizine, but the sample size was under 100. And ‘magnesium helps’? That’s a 2003 study with no control group. This reads like a blog post disguised as medical advice. Where’s the double-blind RCT data?
matthew martin
February 6, 2026 AT 14:41Man, I used to think I was just ‘clumsy’ or ‘anxious.’ Then I started noticing the pattern - dizziness after sleep deprivation, or when the barometric pressure dropped. I kept a journal like this guy said. Turned out my trigger was dark chocolate (tyramine, lol). Cut it out. Started doing 10 minutes of head movements every morning. Now I’m not scared to turn my head in the shower. This isn’t just info - it’s freedom.
Chris Urdilas
February 7, 2026 AT 06:53So… you’re telling me I don’t need to quit my job, move to a cave, and stop breathing? 😏